TRIAGE
Emergency Medical Services: A Systems Study
The purpose of this research was to gain insight into the working of the Indian Emergency Medical Services (EMS) through a systems approach, thereby identifying the problem areas that may need improvement and change.
Process
The goal was to map the functioning of EMS in India.
This was done by:
1. Studying the existing EMS systems across the globe and in India.
2. Creating a benchmark for
comparison from the research findings.
3. Comparing the current state of
Indian EMS against the benchmark
to identify problem areas.
This process led to the finding that while there is a National policy on EMS in place, in reality the system is fragmented in its functioning.
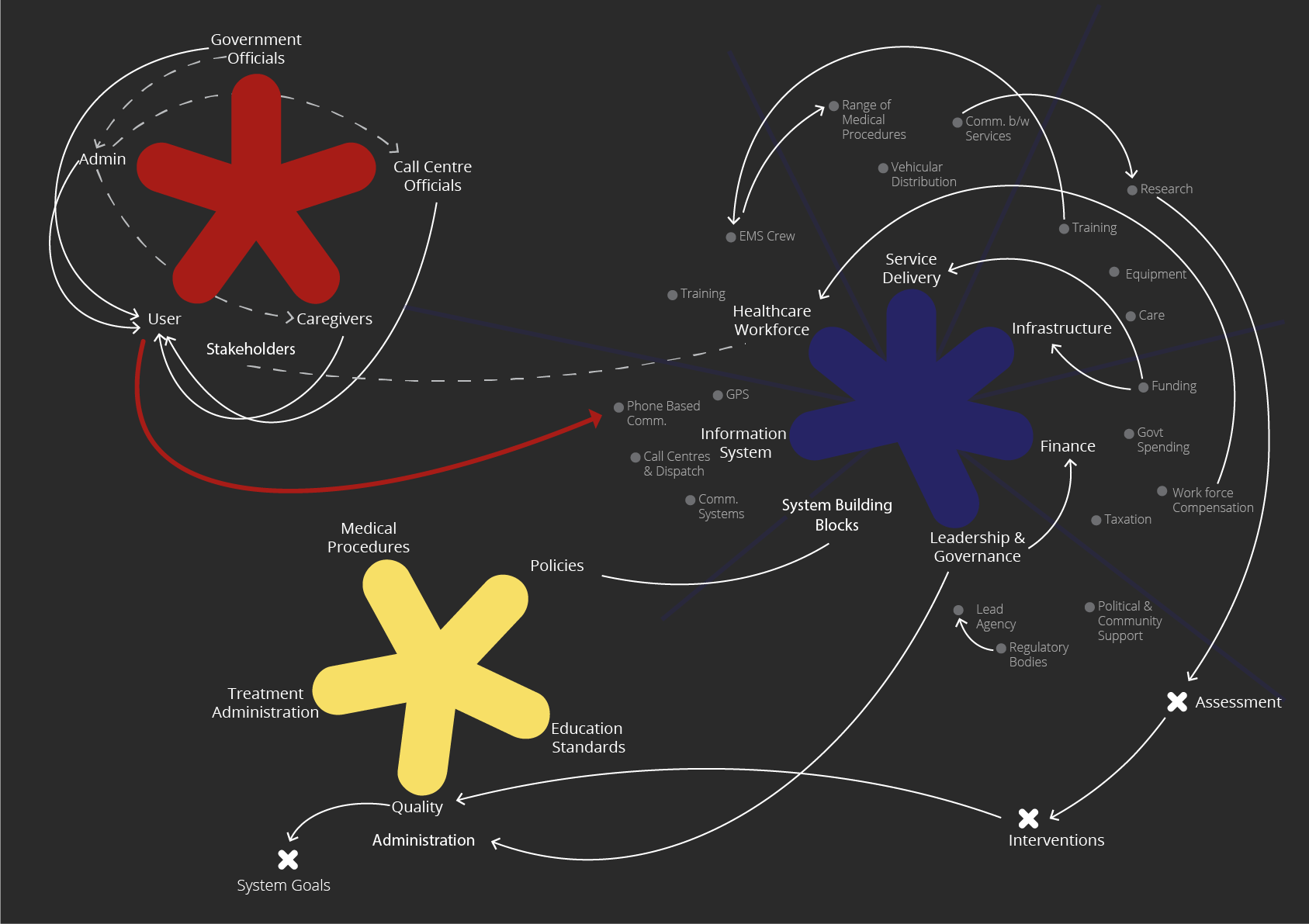
A conceptual benchmark was developed using WHO guidelines on emergency care and research to compare the existing model against, identifying where the system is effective and where it falls short. Key system elements were identified and grouped by function, forming clear structural categories that help visualize their connections. This conceptual framework would rely on the interconnectedness of:
Health Service Delivery Model, trained EMS Workforce, well-functioning Communication Systems, Access to equipment, medicine, procedures, and transport, appropriate use of Technology by staff, Financing mechanisms to sustain EMS, Leadership and Governance to define policies
Systems Analysis
Map Breakdown
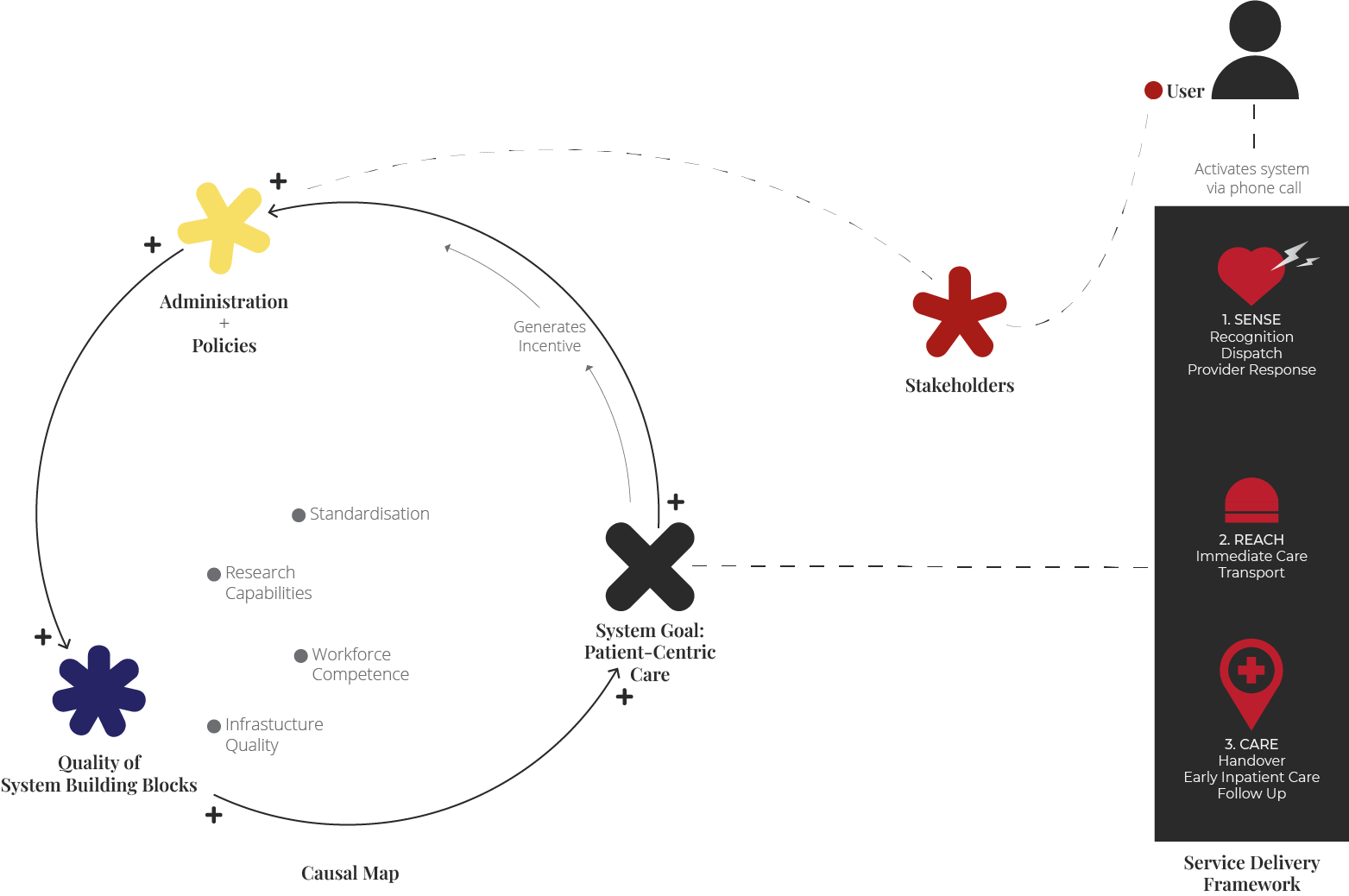
The ethical obligation of all stakeholders is to the user. Policies affect all system building blocks and drive the service forward. Better policies imply improvements in infrastructure and training capabilities, developing a more resilient EMS workforce. Additionally, better policies lead to standardisation across the country, making quality assessment more efficient, in turn generating more accurate insights and propelling policy improvement further. This reinforces the loop and ensures optimal patient-centric care.
The goal of the EMS system is to provide patient-centric care, and policies have the greatest effect on the system’s functioning. This is where the Indian EMS is currently lacking. Adoption of a joint centre-state legal and regulatory framework would reduce technical, legal, and administrative variations in the organisation and delivery of publicly financed EMS. There is no standardised practice amongst the services in each state, and this, paired with severe employee dissatisfaction, only results in a failing system.
There are gaps in the design and management of contracts of EMS due to the peculiar nature of EMS, poor contract design, and governance, leading to severe principal-agent problems. Currently, there is a pressing need for:
A centralised medical emergency authority
Standardised practice
Reduction of employee satisfaction
Changes at operational level
Health information gathering
Service Transparency
Facilities for EMS education
Insights
A.02 Triage, 2019Reflections, 2025